Abstract
Background Tyrosine kinase inhibitors (TKIs) have significantly improved the prognosis of patients(pts) with Ph/BCR-ABL1-positive (Ph/BCR-ABL1+) acute lymphoblastic leukemia (ALL). However, mutations in the ABL1 kinase domain, especially T315I, are the main mechanism of resistance to the first- or second-generation TKIs. Olverembatinib is a novel third-generation TKI developed in China and approved in Dec. 2021, which has been demonstrated great efficacy and safety in clinical trials of CML with T315I mutation. Our study is the first application of Olverembatinib in adult Ph/BCR-ABL1+ ALL with T315I mutation. Herein, we report the preliminary results.
Methods In this exploratory study, adult Ph/BCR-ABL1+ ALL pts with T315I mutation or disease progression were treated with olverembatinib monotherapy (40 mg, every 2 days) or in combination with VP based low intensive chemotherapy (Vincristine/Prednisone) in our institution. Efficacy was assessed by complete remission (CR) rate, MRDneg (<0.01%) rate by multiparameter flow cytometry (MFC) and CMR (BCR-ABL1 transcript<10-5) rate by real-time quantitative polymerase chain reaction (RT-qPCR). Safety profiles were also monitored in this study.
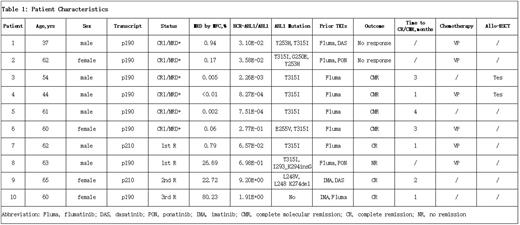
Results From December 2021 to June 2022, 10 Ph/BCR-ABL1+ ALL pts were treated with olverembatinib due to T315I mutation or disease recurrence, after prior TKIs combined with chemotherapy. Median age was 60.5 years (range, 37-65), and 6/10 were males. 5 pts had received 2 types of TKIs previously, of which 2 pts relapsed after ponatinib (Table 1). Among 10 pts, 6 were still in CR1 (pt 1-6), their T315I mutations were detected during regular follow-up. 4/6 pts were persistently molecular positive, while the other 2 had molecular relapse. Median time from diagnosis to the administration of olverembatinib was 5 months (range, 3-17). Among the 4 pts with hematologic relapse (pt 7-10), 2 (pt 7, 8) had T315I mutation. Because of the successive occurrence of G250E, Y253H, L248V mutations and L248 K274del, the 3rd one (pt 9) relapsed twice and failed to response to two kinds of TKIs and chemotherapy. As for the last pt (pt 10), although no ABL1 mutations were found, she was in 3rd relapse with CNS and BM involvement. Median time from diagnosis to the start of olverembatinib for these 4 relapsed pts was 28 months (range, 5-41).
Among 6 pts with T315I mutation and persistent molecular diseases or molecular relapse, the CMR rate was 66.7%, with a median time of 3 months (range, 1-4) to achieve CMR. Then 2 pts underwent allo-HSCT (pt3, 4), who were still in CR. Among 4 hematological relapsed pts, the CR rate was 75%. 1 pt (pt8) with T315I was unresponsive, while another T315I positive patient achieved MRDneg by MFC after 1 month of treatment, with a complete disappearance of T315I mutation (pt7), though the BCR-ABL1 transcript was still positive. The remaining 2 relapsed pts without T315I mutation achieved hematologic CR after 1 month of olverembatinib monotherapy (pt9,10). Totally, overall response rate (ORR) was 70% and MRDneg rate by MFC was 71.4% (5/7), while the CMR rate by PCR was 57.1% (4/7). Notably, olverembatinib was ineffective in neither of the 2 pts who have been previously treated by ponatinib.
Meanwhile, the olverembatinib-based therapy was well-tolerated, and the main adverse events of the third-generation TKIs, such as cytopenia, elevated transaminases, hypertension, and cardiovascular events, were less frequent than those reported relating to ponatinib. In addition, 4 patients developed grade 1 skin pigmentation (pt2,3,6,9). There were no drug-related death or permanent discontinuation due to toxicity.
Conclusion This work suggests that Olverembatinib is a very promising 3rd-generation TKI. It is effective and safe in Chinese adult Ph/BCR-ABL1+ ALL with extremely poor prognosis, especially in T315I mutated or relapsed pts.
Disclosures
No relevant conflicts of interest to declare.
OffLabel Disclosure:
Olverembatinib is used for adult patients with Philadelphia chromosome/BCR-ABL1-positive acute lymphoblastic leukemia with T315I mutation and relapsed disease.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal